Sleep Apnea Linked to Lower Stroke Mortality in Research by New York Medical College Students and Faculty
Study finds decreased risk for mortality and in-hospital complications in stroke patients who undergo thrombectomy
New research by New York Medical College (NYMC) students and faculty found obstructive sleep apnea (OSA) to be linked to a decreased risk for mortality and in-hospital complications in stroke patients who undergo thrombectomy. The research, which was recently published as an abstract in the Journal of Neurological Sciences, was conducted under the guidance of Fawaz Al-Mufti, M.D., associate professor of neurology, neurosurgery and radiology, as part of the Summer Research and Clinical Neurosurgery Program, and supported by a NYMC Medical Student Affairs Summer Fellowship grant during the summer of 2020.
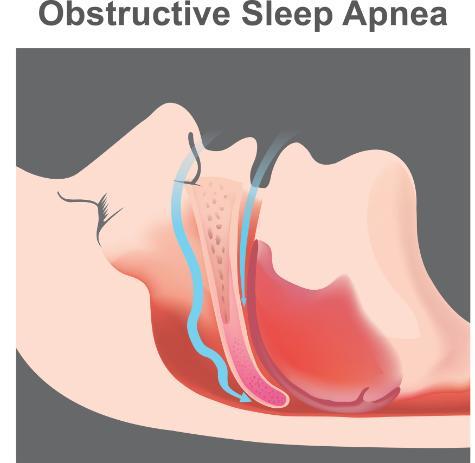
OSA, a common condition characterized by pharyngeal airway collapse causing temporary cessation of breathing during sleep, affects up to 38 percent of the general adult population. Prior studies have found sleep apnea reported in up to 72 percent of stroke and transient ischemic attack patients.
“Previous studies have shown that stroke patients with OSA tend to have poorer outcomes, including higher short-term mortality, diminished long-term functional outcomes and increased risk of recurrent stroke,” said Justin Lapow, School of Medicine (SOM) Class of 2023, who served as lead author of the study and recently presented the findings at the virtual meeting of the XXV World Congress of Neurology (WCN).
Currently, intravenous thrombolytic therapies, such as tissue plasminogen activator (tPA), along with mechanical thrombectomy (MT) are mainstays in the treatment of acute ischemic stroke (AIS).
“To date, no studies have examined the outcomes of OSA patients treated with MT for AIS,” said Mr. Lapow. "Our goal was to determine whether the use of MT as a definitive reperfusion therapy could reduce the disparity in outcomes often observed in OSA vs non-OSA AIS patients.”
The study utilized the National Inpatient Sample (NIS) to conduct a cross-sectional analysis of more than 100,000 patients with AIS treated with MT from 2010 to 2018. The NIS is the largest inpatient database in the United States, representing 20 percent of all US community hospital discharges annually.
“Interestingly, we found that those with OSA suffered from a lower in-hospital mortality than those without OSA after treatment with MT,” said Mr. Lapow. “This association persisted even after accounting for the presence of obesity, severity of illness and other comorbidities, such as hypertension, diabetes and atrial fibrillation in our multivariable analysis. These results differ from a multitude of previous studies that have shown stroke patients with OSA are at an increased risk for mortality. The rate of intracranial hemorrhage was also lower among the OSA group than the non-OSA group.”
“One possible explanation for our results is that those with OSA undergo ischemic preconditioning in the brain that then allows for an increased tolerance to the disruptions that occur during a stroke.”
“This project is the first that I have led from start to completion and has been incredibly formative in my development as a researcher,” said Mr. Lapow. “I not only learned about the process of taking a project from an idea to a full manuscript but also how research findings can then be disseminated through presentation at research conferences. It has been incredibly gratifying to see how something that started as a simple research question can blossom into something so much greater. Having the opportunity to present this work at the World Congress of Neurology was truly an honor.”
